Total Hip Replacement
The first step when making the decision about hip replacement is to meet with your surgeon to see if you are a candidate for total hip replacement surgery. Your surgeon will take your medical history, perform a physical examination and X-ray your hip. Even if the pain is significant, and the X-rays show advanced arthritis of the joint, the first line of treatment is nearly always non-operative. This includes weight loss if appropriate, an exercise regimen, medication, injections, or bracing. If the symptoms persist despite these measures, and with corroborating X-rays, then you may consider surgery.
The decision to move forward with surgery is not always straight forward and usually involves a thoughtful conversation with yourself, your loved ones and ultimately your surgeon. The final decision rests on you based on the pain and disability from the arthritis influencing your quality of life and daily activities. Those who decide to proceed with surgery commonly report that their symptoms keep them from participating in activities that are important to them like walking, taking stairs, working, sleeping, putting on socks and shoes, sitting for long periods of time. Surgery is the next option when non-operative treatments have failed. Below are answers to the most common questions about total hip replacement surgery.
How long does it last?
A common reply to this question is that total joint replacement lasts approximately 15-20 years. A more accurate way to think about longevity is via the annual failure rates.
Most current data suggests that both hip and knee replacements have an annual failure rate between 0.5-1.0%. This means that if you have your total joint replaced today, you have a 90-95% chance that your joint will last 10 years, and a 80-85% that it will last 20 years. With improvements in technology, these numbers may improve.
Despite such improvements it is important to maintain long-term follow-up with your surgeon to assure your replacement is functioning appropriately.
Are all hip replacement implants the same?
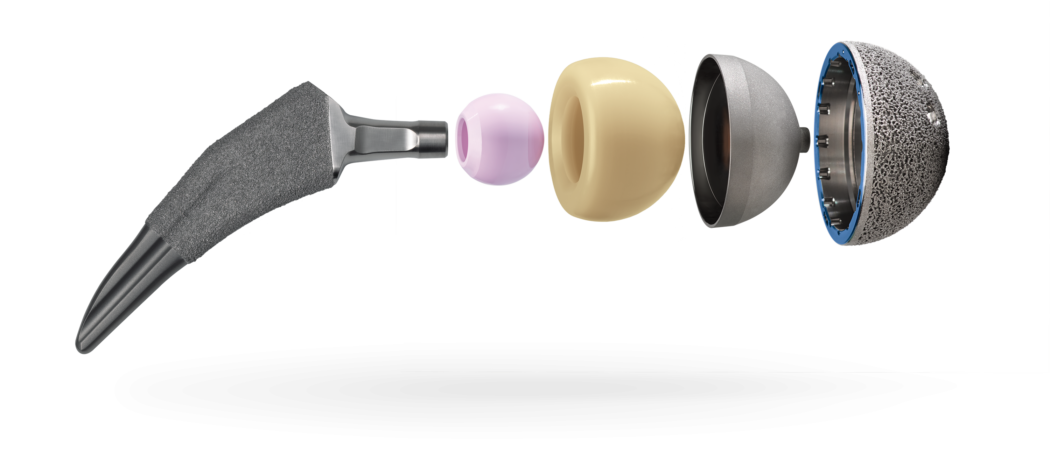
Most implants today have become more similar than different as surgeons and manufacturers have determined which designs work best. One variable that still remains is the bearing surface. The bearing surface is the ball and liner that attach to the stem and cup that fix to the bone.
The ball can be composed of either metal (cobalt chromium alloy) or ceramic, and the liner can be made of plastic (polyethylene), metal, or ceramic. The ball and liner can then be used in different combinations and are named for the respective ball liner combination (metal on poly, ceramic on poly, ceramic on ceramic, etc.).
In 2015, the vast majority of bearings utilized a polyethylene liner with either a metal or ceramic head, with other combinations being used with less frequency. You can discuss these differences with your surgeon to determine which implant is best for you.
Is surgery and recovery very painful?
Pain following total hip replacement has come a long way over the last 10-15 years with increased use of regional nerve blocks, spinal blocks, and various other modalities used for pain control. Total hip replacement is generally considered to be less painful than total knee replacement. Early range of motion and rapid rehabilitation protocols are also designed to reduce early stiffness and pain, making the procedure in general much less painful than in years past. You may have relatively mild pain following the procedure, or you may have a more difficult time than others. Everyone is unique and handles and perceives pain differently. Keep in mind that while pain management has greatly improved, a pain-free surgery is unlikely. You will want to take your pain medicines as directed by your surgeon.
What is minimally invasive surgery?
Minimally invasive surgery is a term that describes a combination of reducing the incision length and lessening tissue disruption beneath the incision. This includes cutting less muscle and detaching less tendon from bone. There have also been advancements in anesthesia and pain management during and after surgery. All of these practices allow you to feel better, have less pain, and regain function faster than in the recent past. While there may be some early advantages to minimally invasive surgery, as long as the components are placed correctly, traditional surgery ultimately leads to similar outcomes by three months post-operatively.
My surgeon talks about “approach.” What is this?
The way a surgeon gains access to the hip during hip replacement surgery is referred to as an “approach.” There are various types of approaches named according to the direction that the surgery is performed.
The most common approach today is referred to as the “posterior approach,” which is done from the back of the hip. Some more recent improvements to this approach (small incision and less tissue trauma) have been called “mini posterior approach.” Another currently popular approach is known as the “anterior approach,” which is performed from the front of the hip. The lateral approach is less frequently used but a viable approach for the surgery.
There are pros and cons of each approach and little science to endorse one over the other. Surgeons tend to have a preference and comfort level with one particular approach over the others. The bottom line is that the best approach is the one your doctor is most comfortable with to allow safe and precise implantation of your hip replacement components. A conversation with your surgeon should help decide which approach is best for you.
Will my surgeon use a computer, robot, or custom cutting guide in my surgery?
There are many studies attempting to evaluate these emerging technologies and their influence of the success of surgeries. Each of these technologies has a specific goal that has fueled its development (i.e. more accuracy in implant placement, more efficient or faster surgery, etc.).
To date, there appears to be both pros and cons to each of these technologies without any clear advantages, but more research is required to determine what advantage, if any, these may offer.
Despite a substantial amount of direct-to-consumer marketing, the best approach is to discuss this topic with your surgeon. You may want to know if they use one of these technologies, why they have chosen to do so, and what their experience has been in using it.
Here are LPSM / ADK Joint Surgery your surgeon has access to CAD technology to pre-plan the best choice and fit of implant to your specific needs and anatomy. For more info click: Introducing CAD Design.
How big will my scar be?
The size of the incision can vary and depends on several factors that include the size of the patient, the complexity of the surgery, and surgeon preference. Most studies have shown that smaller incisions offer no improvement in pain or recovery and may actually worsen the surgeon’s ability to adequately perform the procedure.
Will I need general anesthesia?
While general anesthesia is a safe option, both hip and knee replacements can be performed under regional anesthesia. Choices for regional anesthesia include spinal anesthesia, epidural anesthesia, or one of a variety of peripheral nerve blocks. Many surgeons and anesthesiologists prefer regional anesthesia because data shows it can reduce complications and improve your recovery experience with less pain, less nausea, less narcotic medicine required, etc. Recently, peripheral nerve blocks have become more popular as an adjunct for pain control. For total knee replacement this can include an adductor canal block, which allows pain control without causing weakness of your muscles. You should have a discussion regarding anesthesia and post-operative pain management with your surgeon and anesthesia team prior to your surgery.
How long will I stay in the hospital?
You will likely stay in the hospital for one to three days depending on your rehabilitation protocol and how fast you progress with physical therapy. This is highly dependent upon your condition before surgery, your age, and medical problems which can influence your rehabilitation. A safe discharge plan will be arranged for you by the orthopaedic team.
How long does it take to recover?
The majority of people who undergo total hip replacement are able to participate in a majority of their daily activities by six weeks. By three months, most people have regained much the endurance and strength lost around the time of surgery, and can participate in daily activities without restriction. While daily activities have resumed, it is important to avoid high impact activities to give you the best long-term outcome with your hip.
When can I shower?
Most surgeons do not like the wound to be exposed to water for five to seven days; however, more surgeons are using waterproof dressings that allow patients to shower the day after surgery. You can remove the dressing at seven to ten days after surgery. Once you remove the dressings, you still shouldn’t soak the wound until the incision is completely healed three to four weeks later. Either way, it is important to discuss this with your surgeon to be assured when it is safe to shower and what wound closure technique/dressings will be used for your surgical wound.
When can I walk after surgery?
Most surgeons and hospitals today emphasize getting you out of bed quickly. Most people are walking with the assistance of a walker on the day after surgery. Early ambulation has been shown to reduce the risk of a post-operative blood clot and is an important part of your recovery. Progression to using a cane or nothing at all typically occurs within the first month or two after surgery and depends on each individual’s progress. Despite the rapid progression to moving without assistance, it is typically not recommended that you return to sporting activities until the third month after surgery.
When can I drive?
Most surgeons allow patients to drive at four to six weeks after surgery, and sometimes sooner if the operative leg is the left leg. There is some literature that states that your reaction time will not be back to normal prior to six weeks. You should not drive while on narcotics, and should discuss returning to driving with your operating surgeon.
When can I return to work?
Returning to work is highly dependent on your general health, activity level and demands of your job. If you have a sedentary job, such as computer work, you can expect to return to work in four to six weeks. If you have a more demanding job that requires lifting, walking, or travel, you may need up to three months for full recovery
What restrictions will I have after surgery?
Depending on how your surgeon performs your surgery, you may have slight differences in your rehabilitation instructions including restrictions. In general most surgeons prefer that you avoid certain positions of the hip that can increase your risk of dislocation of the hip for about six weeks following surgery. After six weeks, the soft tissues involved in the surgery have healed, and restrictions are often lifted – allowing more vigorous activity.
Many surgeons suggest that you avoid any repetitive impact activities that can increase the wear on the implant such as long distance running, basketball, or mogul skiing. Otherwise limitations following hip replacement surgery are few; however, the better you treat your replacement the longer it will last.
Will I need physical therapy, and if so, for how long?
Initially, you will receive some physical therapy while in the hospital. Depending on your preoperative conditioning and support, you may or may not need additional therapy as an outpatient. Much of the therapy after hip replacement is walking with general stretching and thigh muscle strengthening, which you can do on your own without the assistance of a physical therapist.
Are there complications to THR?
- Total hip replacement is an excellent pain relieving procedure, and most patients receive approximately 95% pain relief.
- Although complications are relatively rare (1-5% of patients), patients may experience a complication in the postoperative period. These include very serious and possibly life threatening complications such as heart attack, stroke, pulmonary embolism and kidney failure.
- Infection (1%) is one of the most debilitating complications and often requires prolonged antibiotics with several additional surgeries to rid the infection.
- A blood clot in the leg is also a relatively common complication requiring some type of blood thinner following surgery to reduce the incidence.
- The implants used can also fail over time due to wear of the bearing components or loosening of the components from the bone, both of which usually occur over many years.
- Another complication specific to hip replacement is dislocation of the joint (1%) that may require additional surgery if dislocation becomes recurring.
- Leg length differences following surgery are also a possibility and may be difficult to avoid sometimes in order to insure a stable hip. Often this leg length discrepancy is mild are rarely needs treatment.
Living with Your New Joint
Will my implant set off metal detectors at airports and courthouses?
Usually patients with joint replacements will set off metal detectors. It is reasonable for you to inform the TSA screening agent at the airport that you have had a joint replacement; however, you will still require screening and will need to follow the directions of the screening agent. Learn more about airport security.
There are millions of individuals with joint replacements, and screening protocols recognize that people who have had joint replacements may set off detectors. You do not need to carry specific documentation to prove that you have a joint replacement.
Metal detector screenings follow universal protocols that allow for people with joint replacements to proceed after confirmation that no threat exists.
Will I need to take antibiotics prior to seeing a dentist or having other invasive procedures?
The American Academy of Orthopedic Surgery (AAOS) and American Dental Association (ADA) have generally recommended short-term antibiotics prior to dental procedures (one dose one hour prior to dental procedure) for patients who have had joint replacements. This recommendation continues for up to two years after your joint replacement.
Two or more years after the replacement, continued use of antibiotics prior to dental procedures is based on the discretion of the treating surgeon and the patient. Your surgeon will consider many factors including whether or not you are at increased risk of infection due to immune suppression (i.e. diabetic, transplant patients, and rheumatoid arthritis).
The use of prophylactic antibiotics prior to dental cleanings and other invasive procedures remains controversial. Most orthopaedic surgeons now recommend lifetime suppression. Patients should discuss whether or not they need antibiotics prior to dental or other invasive procedures with their treating orthopedic surgeon. See also “Preventing Infection in Your Joint at the Dentist’s Office.”
Source
This article has been written and peer reviewed by the AAHKS Patient and Public Relations Committee and the AAHKS Evidence Based Medicine Committee. Links to these pages or content used from the articles must be given proper citation to the American Association of Hip and Knee Surgeons.